This is a reading test of Vilaweb articles in a synthetic voice, which will soon be available to newspaper subscribers. Subscribe here. If you encounter any problems, write to us at [email protected].
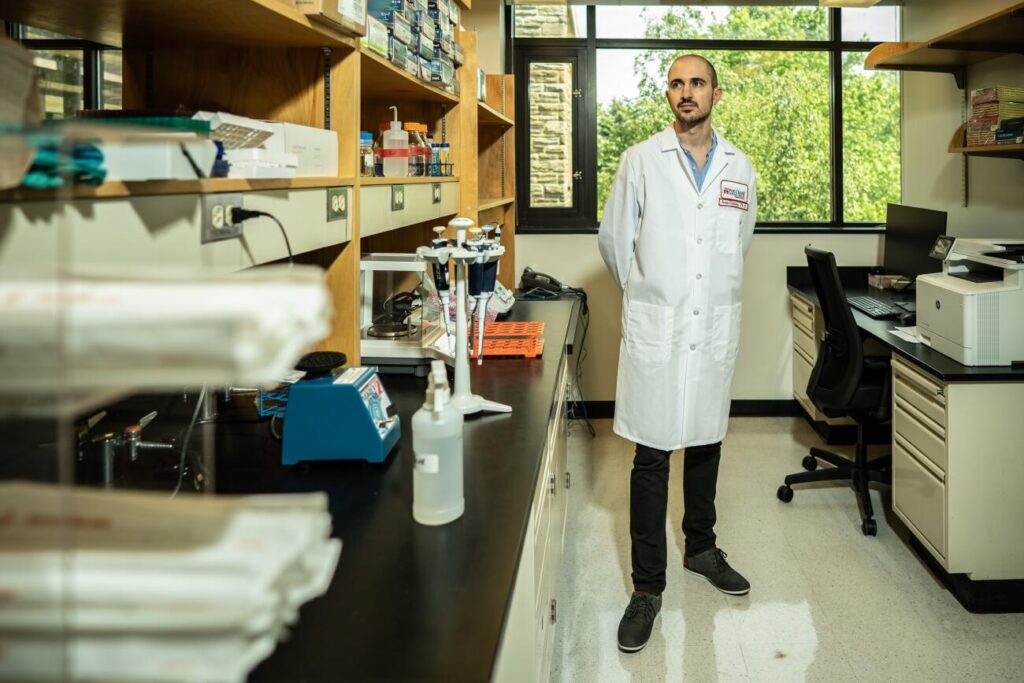
Catalan world Israel CanadaHe, who leads his own group at the Fox Chase Cancer Center in Philadelphia (USA), has found a mechanism to activate the immune system to attack tumors that have managed to “hide.” In a study in preclinical models published in the journal Cancer Discovery, researchers describe a strategy that significantly improves response Immunotherapy in lung cancer Of small cells, very aggressive and almost always associated with tobacco. The process involves blocking a gene so that there appears to be a viral infection and the immune system is activated. In an interview with ACN, Cañadas points out that the mechanism, called viral mimicry, is now a hot topic in cancer research.
The strategy has been tested in the laboratory so far, and the plan is to start a clinical trial in patients soon to evaluate the treatment's effectiveness and safety. Dr. Cañadas says the results so far are promising, and he hopes that if this and other treatments in development eventually reach patients, prognosis for small cell lung cancer could be improved.
This type of tumor represents 15% of diagnosed lung cancers, and its survival rate after five years is very low. Therefore, achieving a breakthrough in this field is a great hope.
Getting a tumor “cold” to respond to immunotherapy
Immunotherapy, a group of treatments that helps the immune system fight cancer, has revolutionized oncology research for more than a decade. “In the end, the immune system is the most powerful and specific mechanism capable of detecting cancer cells,” this scientist said from his office in Philadelphia after publishing the study in the famous journal “Cancer Detection.”
Cañadas' group describes a mechanism for converting a “cold tumor”—a tumor that is likely to have a low immune response—into an immunologically “hot” tumor. Cells in “cold tumors” find strategies to avoid immune attack or even find mechanisms to avoid entry by immune cells. “The immune system is programmed to attack tumors, but the ‘cold tumors’ have managed to hide themselves,” Cañadas explains.
Researchers have studied these tumors genetically to determine strategies to increase their immune response. Through gene editing techniques, Canidas' group discovered a gene in cancer cells, DHX9, whose function is to inhibit double-stranded RNA (a feature of some viruses). Researchers have observed that if this gene is blocked, double-stranded RNA accumulates within the cell and the immune system is activated. This process is known as viral mimicry.
Imitating the virus to activate the immune system
In the face of infection, the body's cells have mechanisms to recognize the dsRNA of the virus genome and activate the immune system to destroy it. With the ablation of the DHX9 gene and the accumulation of dsRNA, “the immune system is activated as if the cells were infected with a virus, but without them being,” Cañadas explains.
In vivo, the researchers observed that tumor growth was significantly reduced and, at the same time, it was more permeable to immune system cells. “The tumor practically disappeared and the survival rate in the mice increased significantly. The effect was very pronounced, and it indicates that combining DHX9 gene inhibitors with immunotherapy in the future will be very promising for attacking tumors.”
Cañadas's lab first blocked the gene using the CRISPR gene editor, but later, in collaboration with the Massachusetts pharmaceutical company Accent Therapeutics, developed a drug that inhibits DHX9. Cañadas points out that Fox Chase Cancer Center, also a hospital, is very interested in translational research aimed at applying it to clinical practice, so the plan is to start a clinical trial soon. In addition, this strategy is also a promising route for other types of “cold” tumors.
From Baix Llobregat to the forefront of medicine
Canidas, from Prat de Llobregat, has focused his research on cancer immunology, specifically lung cancer, and immunotherapy. After studying biology at the University of Barcelona and doctoral studies in biomedicine at the Pompeu Fabra University and the IMIM-Hospital del Mar Research Institute, he moved to Boston to do a postdoctoral residency at the Dana-Farber Cancer Institute – Harvard Medical School, where he featured these viruses in a study published in Nature Medicine about a new subclass of endogenous retroviruses that activate innate immunity in cancer cells. In early 2020, he started his own research group at Fox Chase Cancer Center in Philadelphia.
This center, founded in 1926, has been home to some great discoveries in cancer prevention and treatment. One of the most famous of these discoveries is the identification of the “Philadelphia chromosome,” a discovery that led to current treatments directed against leukemia.
Fox Chase Cancer Center also witnessed the discovery of the hepatitis B virus and the development of its vaccine, a discovery that won a Nobel Prize for its CEO, Baruch S. Bloomberg. In addition, fundamental progress has been made in reprogramming cancer cells or understanding genetic risks for cancer, among others.

“Infuriatingly humble social media buff. Twitter advocate. Writer. Internet nerd.”